Overcome Your Denials With Strategy
With nearly 30% of clams being denied pre and post billing, it’s time to have predictive solutions with tangible results
Stunning Facts That Impact You
1 5
Increase in Denials
Providers nationwide are seeing an increase of up to 15% in denials post-COVID
25
More Money Less Results
Practices are spending up to $25 per claim and hospitals up to $180 to resolve denials
26
New Audit Targets
This year alone there have been 26 new audit targets for healthcare professionals
What Are Your Options?

Pre-Bill
A prebill denial review will allow you to catch when the claim may be potentially denied and address the billing or coding concerns proactively resulting in lower denial rates with payer

Post-Bill
Post bill occurs when you have submitted the claim for reibursement yet the payer has denied all or some of the cliam charges requiring you to go back and rework the claim

Predictive
Predictive denial analysis is when you can predict today, your future denials thus allowing you to not only address such proactively but plan for your financial future
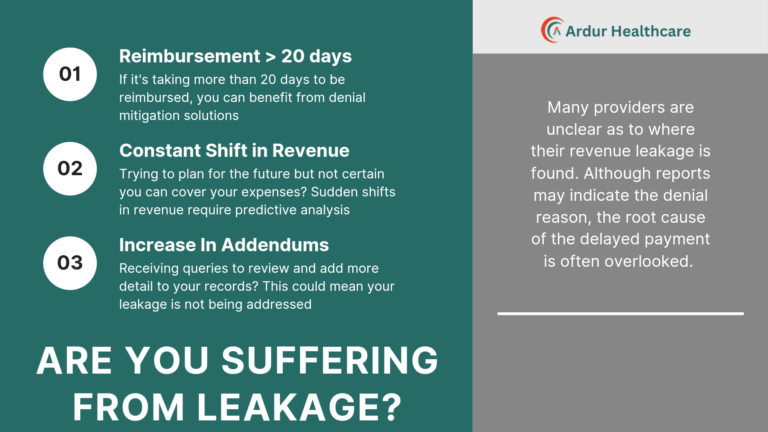
Are You Trapped?
Providers are now utilizing more technology to help prevent and mitigate denials resulting in faster reimbursement times and fewer human error concerns. Those who are not adapting such technology are consistently being targeted by payers causing a never-ending reimbursement nightmare.